'Nothing you can do' - Older patients 'no longer feel protected'
 BBC
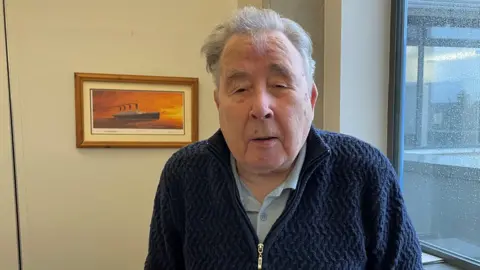
BBCAn elderly man who spent "a couple of weeks" in a hospital corridor after suffering a stroke has spoken of the frustration older patients experience in the health system.
Andy Leebody, who is 87, said if a hospital does not have the bed space on a ward for you, there is "nothing you can do about it".
He was speaking after Northern Ireland's Commissioner for Older People, Siobhan Casey, claimed elderly people "no longer feel protected" by the health service.
She has published a new report examining how current pressures on the health service are being experienced by older people, with many describing barriers to accessing GPs, emergency treatment , hospital care and social care.
The report said that demand for health and social care is growing faster than the system's capacity to respond.
Casey described how winter pressures are now a year-round reality, "driven not by temporary post-Covid disruption, but by irreversible demographic change".
'You have to just lie there and that's it'
Leebody explained that when he was in hospital after his stroke, he spent "a couple of weeks" lying on a bed in a corridor because the wards were full.
"If they haven't got the space to take you, there's nothing you can do about it.
"You have to just lie there and that's it," he told BBC News NI.
However, the pensioner said although he could not get into a ward, the staff took good care of him during his time in hospital.
Leebody also expressed hope that the current situation could improve.
The Department of Health was asked for a response to the report from the Commission for Older People for Northern Ireland (COPNI).
Patient called GP '300 or 400 times'

Another patient - Eddie - told BBC News NI about the problems he experiences when trying to access GP services.
He said he sometimes he has to call his family doctor "three or four hundred times" to get through to someone.
"Then when I eventually do get through, they turn round and tell me there's no appointments," he continued.
Eddie also expressed frustration at not getting to see a doctor face-to-face.
"How can you examine somebody on the phone and know what's wrong with them?
"You need to see a doctor and that is almost impossible nowadays."
'It's going to get worse without reform'

The access issues faced by the older generation are a problem for the whole of society, and any younger people who believe this doesn't affect them are "wrong", according to Casey.
"We are all ageing," the commissioner said.
"The system we allow to decline today is the one we will all rely on tomorrow."
She stressed the need for a whole government approach.
Casey added that she has a "lot of hope" and called for the Stormont executive to support the Department of Health and enact the change that's needed.
"It's going to get worse unless we can get the reform," she said.
Speaking on BBC Radio Ulster's Good Morning Ulster, the commissioner described hearing how people are having to ring 100 times to get a GP appointment.
She said the number of phone calls causes "anxiety, stress and a feeling of worthlessness".
Casey said the issue of health care access is "a difficulty" that has to be acknowledged.
"We've got a 100,000 more older people than we did 10 years ago," Casey said.
But she added there are fewer GPs, fewer social care packages, fewer care home beds and longer waiting lists.
'The current situation is not sustainable'
Dr Alan Stout, who chairs the British Medical Association's (BMA) Northern Ireland Council, agreed that access to hospital care takes too long and some unacceptable waits are now routine.
However he said access problems are not due to GPs or practice staff but were the "consequence of sustained and growing pressures on general practice".
He explained those pressures arose from "years of underfunding" combined with rising need from an ageing population, fewer GP practices, larger patient lists and workforce shortages.
Stout explained that many practices have adopted telephone and triage systems because it is the only way to manage demand.
"The current situation is not sustainable," he said.
He added what is needed is a "clear, long‑term plan to stabilise and invest in services, support and retain the medical workforce, and match capacity to population need".