What really causes migraines?
 Serenity Strull/ BBC
Serenity Strull/ BBCOur understanding of migraine disorder is finally starting to shift, overturning ideas of what's a symptom and what's a trigger, and which part of the brain is key for developing effective treatments.
About twice a week, the left side of my head starts to feel like there's a bit too much space between my brain and my skull. When I tilt it, that space fills up with a dull, liquid pain. The pain creeps behind my eyeball, where it sits like a dagger, and then treads down all the way to my jaw. Sometimes it burns and rings in the back of my mind if I squint. On other occasions, it pulses and thuds, as if knocking and asking to come out.
The more I let the pain run wild before I take my medication, the longer it'll take to tame it, and the more likely it'll come back as soon as the effects of the pills wear off. It's a migraine.
More than 1.2 billion people worldwide will be able to relate to some version of my experience. This neurological condition is the second most prevalent cause of disability in the world. Yet, despite its common occurrence and debilitating effects, migraine still remains largely a mystery.
There are many unanswered questions about what migraine actually is, what causes it, and what can be done to eradicate the condition from patients' lives.
"I would say that it's probably among the most poorly understood neurological disorders, or disorders in general," says Gregory Dussor, chair in behavioural and brain sciences at the University of Texas at Dallas, in the US.
Now, researchers are starting to unravel what causes migraine and have even recently been able to see one unfold in real time as electrical signals in the patient's brain. By carrying out studies on genes, blood vessels and the molecular cocktail swirling around in patients' heads, scientists are inching closer to understanding why migraine occurs, how it can be treated and why – far from being a pesky headache – it is a chronic, whole-body experience.
Why it is so hard to study migraine
Starting in the 18th-19th centuries, migraine was typically branded a feminine whim: one that would strike only clever, charming and beautiful women with "migraine personalities". While three-quarters of migraine patients are female, this centuries-long stigma has held back research on migraine and meant it has been chronically underfunded.
"People thought of it as a disease of hysteria," says Teshamae Monteith, chief of the headache division at the University of Miami Health System, in the US. Even today, very few universities have solid migraine research centres and investments into the issue pale compared with the fields of some other neurological conditions.
Migraine language
Experts no longer use the term "migraines" – as if the headaches are the condition. Instead, they now urge everybody to use the term migraine disorder instead, and refer to "migraine attacks" as a flare-up of the underlying ailment, which presents with a variety of symptoms, including headache. Episodic migraine is when a patient gets fewer than fifteen headaches a month. Chronic migraine is when they have more.
Yet the psychological, physical and economic burden of migraine is very real, says Monteith. While migraine is most common during a person's most productive years of life, between mid-twenties and mid-fifties, people with migraine are more likely to have to skip work, lose their jobs and have to retire early. Data from the UK suggests that a 44-year-old with migraine costs the government £19,823 ($27,300) extra each year compared with someone without migraine, meaning that migraine costs £12bn ($17bn) to the public economy overall each year.
One of the challenges of studying migraine is just how wide-ranging the symptoms can be.
Like most people affected by migraine, I am a woman of childbearing age. Attacks are a staple of my life when I get my period. My headache usually hits my left side and gets worse with movement. It is preceded by a strong sensitivity to smell and sometimes my left shoulder and arm feel frozen.
But other patients experience symptoms including nausea and vomiting, vertigo, stomach pain, and heightened sensitivity to light and sound. More than half of patients experience extreme fatigue, while some get specific food cravings. Others find themselves yawning excessively in the early phases. About 25% of patients get auras, visions of jagged bright glares or blurs like film camera light leaks.
"The entire migraine attack is a very complicated thing," says Dussor. "It's not just pain. It's a whole series of events that are happening well before a headache ever starts."
The triggers that are thought to ignite an attack are just as varied: lack of sleep and fasting definitely spark my headaches, but other patients point to chocolate, aged cheese, coffee or white wine spurring theirs. Stress seems heavily intertwined with migraine for the majority of patients, and, interestingly, so is the release of stress – hence why weekend attacks are a classic.
Triggers v symptoms
While scientists studying migraine have long been puzzled by the sheer vast array of diverse triggers, now a growing body of research suggests many of these triggers might instead just be manifestations of early symptoms.
A patient might actually be subconsciously seeking certain foods in those very early stages of an attack – chocolate or cheese, for example. This means it's easy to associate eating that food as a trigger of the attack, but the attack might have already started, says Debbie Hay, professor of pharmacology and toxicology at the University of Otago in Dunedin, New Zealand.
 Serenity Strull/ BBC
Serenity Strull/ BBCPersonally, I've always wondered whether perfume was responsible for giving me a migraine attack. Yet I wear perfume every day, and I realise, I only notice its scent enough to try to blame it for my attack on the days when I actually do get one. If I don't get a migraine attack, I don't tend to focus on what I smell like too much.
"Well, that's a classic example, and the causal attribution is probably wrong," says Peter Goadsby, professor of neurology at King's College London, in the UK. "What if, instead, during the premonitory phase of an attack, you're sensitive to scent, you notice smells that you wouldn't normally."
Goadsby has analysed the brain scans of migraine patients who feel that light triggers their attack and compared them to patients who don't tend to blame light for the onset of their pain. Only the former had overactivity in the part of the brain responsible for vision right before their migraine, suggesting that, during that moment, they were biologically primed to be more sensitive to light than their counterparts. "Unquestionably, something is going on biologically," says Goadsby.
But the quest to discover what that underlying biological mechanism has been a long one.
The genetic origin of migraine
Studies on twins show that there is a strong genetic component and that if your parents or grandparents had migraine, you're statistically likely to inherit the neurological condition too. Inherited genes appear to play a role in an estimated 30-60% of people who suffer from migraine, with other cumulative external factors such as life history, environment and behaviour accounting for the rest, says Dale Nyholt, a geneticist at Queensland University of Technology in Australia.
Nyholt is screening thousands of people to find the exact genes running amok, but the quest has been "more complex than what we were ideally hoping for", he says. In 2022, he trawled through the genes of 100,000 migraine patients, comparing them with those of 770,000 people who do not have migraines.
He identified 123 "risk Snips" – tiny differences in the code of people's DNA – that were associated with migraine. Now he's running another test with 300,000 migraine patients in the hopes of finding more. He estimates "there are probably thousands".
Nyholt's analysis has already revealed, however, that some of the genetic markers involved in migraine seem to be closely correlated with depression and diabetes, as well as with the size of different structures in the brain. Nyholt suspects there is a "constellation" of ways that these same gene clusters can show up as different conditions in the real world due to the way they affect the brain. (Still, the team has not been able to zero in on any of the specific genes at play in a way that's useful for making medication just yet.)
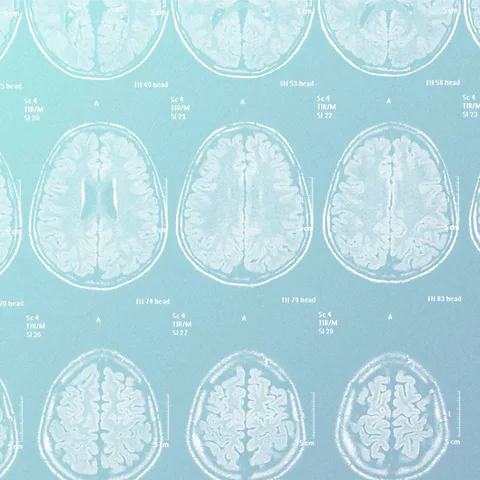 Serenity Strull/ Getty Images
Serenity Strull/ Getty ImagesBlood vs brain
Because of the throbbing nature of many people's headaches, one of the prevailing suspects for migraine attacks used to be blood vessels leading into the brain opening and causing a rush of blood to flood in. But scientists couldn't ever conclusively find a correlation between the blood flow and migraine onset. "It just cannot be as simple as 'blood vessel does X'," says Dussor. "You can give every human on Earth a drug that's going to cause blood vessels to dilate and not everybody's going to get a migraine."
This doesn't mean blood vessels have nothing to do with migraine: many of the risk genes discovered by Nyholt in the genetic test of origins of migraine are genes that help regulate veins. Blood vessels do dilate abnormally during attacks and they can actually be deflated with drugs to help relieve migraine pain. So, while they're definitely involved in a migraine attack, they might not be the cause. Their effects on migraine might be because of other hidden factors, such as an anomalous release of pain-causing molecules in vein walls or other signals being sent from the veins to the brain, says Dussor. Or their dilation could simply be a symptom of migraine rather than a cause.
"Migraine sits at the interface between what people call neurology and psychiatry," says Goadsby. Scientists in his school of thought find correlations between migraine and conditions like seizure, epilepsy or stroke. "The challenge with all the things that really involve the central nervous system is to unpick the parts of it," says Goadsby, from the cellular building blocks of the brain, its structure and how electricity runs through neurons.
Making brain waves
The leading theory for scientists looking at the brain's role in migraine is that an attack is a slow, abnormal electrical wave spreading through the cortex of the brain, known as cortical spreading depression. This wave suppresses the brain's activity and causes nearby pain nerves to fire up, sounding the alarm and triggering inflammation. The cortical spreading depression wave basically "dumps out all kinds of bad molecules into the brain", says Michael Moskowitz, professor of neurology at Harvard Medical School in Cambridge, Massachusetts, in the US.
But why does this rogue wave start? And where does it spread to? And how does this electrical wave lead to so many symptoms? That's still hard to pinpoint. In March 2025, scientists caught the wave in real time while monitoring a 32-year-old patient's brain in preparation for surgery. The wave was picked up through 95 electrodes inserted through her skull. It spread from her visual cortex – which explains why some people have sensitivity to light and visions of auras, says Moskowitz – and then for 80 more minutes throughout the brain.
Migraines
This article is one of a two-part special focus on migraine disorder. Find out about the latest treatments in part two on Friday, 6 February.
The variation in the nature of the wave helps explain why some people just get an aura, others get an aura before a headache and there are those who get a headache before the aura instead, says Moskowitz – it depends on the wave's patterns. But cortical spreading depression still does explain other neurological symptoms that happen during a migraine attack, such as fatigue, yawning, brain fog and cravings for specific types of foods.
Another study involving just a single patient has also suggested that a small region deep inside the brain called the hypothalamus gets strangely activated a full day before a migraine attack. The hypothalamus, after all, is also involved in stress responses and the sleep-wake cycle, which are common migraine triggers. But larger studies are needed to understand its role.
Vitally, however, neither the visual cortex nor the hypothalamus is the location of migraine pain. The headache is felt in the nerve fibres of the meninges – the thick, gelatinous, three-layered outer membrane of the brain – and through a thick nerve bundle called the trigeminal ganglia, which connects the meninges to stimuli from the face, scalp, and eyes. That's why I feel my migraine attack behind my eye socket and all the way to my jaw.
So some scientists believe that this gloopy sack around the brain may hold thekey to understanding migraine instead.
Enter the meninges
The meninges are awash with immune cells whose job is to protect the brain, and when they're excited, the molecules they release can trigger inflammation that can affect the neurons on the other side of the meninges. Dussor and others are bringing forward the hypothesis that an overactive response by these immune cells could be triggering migraine. It might explain why migraine attacks seem to be statistically more common in people with allergic rhinitis and hayfever and anecdotally more prevalent during allergy season, as allergens such as pollen could be setting off these immune cells.
There are other signs that the meninges could be the vital link between the environmental triggers and what then happens in the brain. Dotted along this membrane are structures capable of detecting changes in acidity – which could be caused by physiological fluctuations, inflammation surrounding the brain, or a rogue electrical wave suppressing the brain's activity. When they detect that the meninges become more acidic, they send electrical signals to fire the pain fibres involved in migraine attacks.
Other parts in the meninges respond to heat and the cold in a similar way. This might help to explain why some patients find relief from their headaches with ice packs or hot cushions.
Hormone fluctuations are often seen as culprits too. Many patients report migraine attacks at the onset of their menstrual cycle, and research has shown that a family of molecules known as prostaglandins can have a dramatic effect on the dilation of blood vessels in the brain.
The migraine molecule cocktail
All of these varying factors likely act in an intertwined way. "I think it's that ultimately, there may be one common denominator, but there's multiple paths to migraine," says Amynah Pradhan, director of the Centre for Clinical Pharmacology at Washington University in St. Louis, US. "Maybe even more than that, I think within an individual. There are multiple ways to get migraine and everybody's got a cocktail of things going on."
Still, the search for a standard, objective molecular bioindicator of what makes a brain a migraine brain is not over, and one of the most significant breakthroughs in recent years came from looking for one such molecule. Researchers have identified unusually high levels of a type of neuromodulator called calcitonin gene-related peptides, or CGRPs. These small proteins act like dimmer switches to dial neuron activity and sensitivity up or down. During a migraine attack, there seemed to be higher levels of these, but they also appear to be higher in people who experience migraine even when they are not having an attack, according to research by Goadsby and his team.
This insight has led to new drugs on the market that target CGRPs to either nip an attack in the bud or prevent it, a pharmaceutical advancement that has already relieved a vast population of patients from their pain in ways that other interventions had not. In one October 2025 study looking at over 570 patients on CGRP for a year, 70% achieved a 75% reduction in the frequency of their migraine attacks, and about 23% were rid of migraine attacks completely.
More like this:
• The sexist history of migraines
• How heatwaves affect our brains
• The dementia risk from heading the ball in sport
"It will be great if we can find a molecular marker for migraine, especially as we start patients on treatments and we want to figure out who is a responder and who is not a responder," says Monteith.
But still, the blood measurements that find CGRP surges are mostly reflecting the brain's peripheral mechanisms, says Pradhan. Nobody really knows why CGRPs show up so abundantly in the area of the brain during the attack. They're still likely just small bits of a big puzzle, especially as migraine is increasingly thought of as a spectrum-like, chronic condition that affects the whole body.
"I think there's a lot of opportunities there for people to come in and go dig a little bit," says Pradhan. While this sounds quite daunting – and it doesn't yet dull the pain in my head when an attack comes knocking on a weekly basis – it also makes me feel empowered that science is slowly chipping away at the mystery of migraine, and that though there isn't a one-size-fits-all answer for everybody, there might be a variety of options that come together instead.
"We're just scraping the surface of what's happening with migraine," says Pradhan.
--
For trusted insights on health and wellbeing, sign up to the Health Fix newsletter by senior health correspondent Melissa Hogenboom who also writes the Live Well For Longer and Six Steps to Calm courses.
For more science, technology, environment and health stories from the BBC, follow us on Facebook and Instagram.