Sepsis mistakes killed our daughter - we fear it could happen again
 Steve James
Steve JamesWhen she was 16, Bethan James told her YouTube channel that by 2026 she hoped to have a partner, an enjoyable job and maybe even children.
Bethan would have been 27 now - but her dreams were taken when she died aged 21 from a combination of sepsis, pneumonia and Crohn's disease.
Bethan's sepsis wasn't spotted early enough and life-saving care was delayed. Now her grieving parents are campaigning for better training to diagnose one of the UK's biggest killers.
A BBC investigation has found sepsis awareness training is still not mandatory at most hospitals in Wales, and Bethan's parents fear that what happened to their daughter could still happen to others.
This included at the hospital where Bethan died and the Welsh government said sepsis awareness was a "focus" and a "priority", while the Welsh Ambulance Service said "meaningful changes" had been made.
Jane and Steve James said they were "haunted and totally devastated" by the "needless death" of their eldest child in 2020.
"She was just the kindest, most caring, loving person and she had so much to give," said Jane, from Cardiff.
Steve, a former England cricket international, added: "It just pulls at your heartstrings thinking, where would Bethan be today and what would she be doing?
"We still go about daily things, but underneath there's just this total devastation and so many dark, dark moments. It's a totally abnormal life we live."
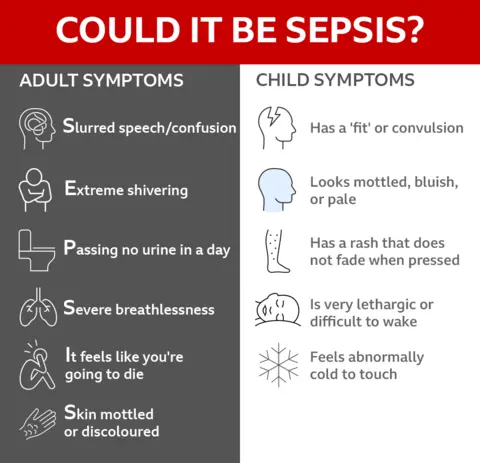
What is sepsis?
Sepsis is a serious complication of an infection.
It develops when the body's immune system overreacts to an infection and starts attacking its own tissues and organs.
The UK Sepsis Trust estimates about 48,000 people die each year from sepsis-related illnesses, "thousands" of which are preventable.
 Steve James
Steve JamesBethan died six years ago this week and her parents fought for an inquest where a coroner found that the journalism student "would not have died" if her care and treatment had not been delayed.
A BBC investigation has found that sepsis awareness training remains a lottery in Wales and is still not compulsory at Wales' largest hospital, the University Hospital of Wales in Cardiff, where Bethan died.
"You go into the hospital and there's sepsis posters on lifts and walls but if their actual frontline staff can't recognise the symptoms of sepsis, it just beggars belief," said Jane.
Bethan was ill in the 10 days before her death and had made five trips to hospital.
"They were just quite dismissive of her symptoms," said Jane, a physiotherapist.
"Her heart rate was high, her blood pressure was low - it was so hard to get them to listen."
Bethan's condition worsened and she returned to hospital days later, where she saw the same doctor.
 Steve James
Steve JamesSteve, now a sports writer for The Times, recalled one medic telling them Bethan would recover soon.
"I was due to go to Ireland to cover the Six Nations rugby game between Ireland and Wales," Steve recalled.
"I was unsure whether to go but [I remember] him saying that he thought she would be OK in two weeks' time," he added.
"Even on the Saturday when she died, [Bethan] kept saying to Jane 'that doctor said I was going to be OK'.
"I went to Ireland. That's a decision I've got to live with the rest of my life - I regret it so deeply, but I just took his word."
 Steve James
Steve JamesA day after Steve left for Dublin, Bethan's condition deteriorated. Jane dialled 999, and a paramedic arrived at their Cardiff home.
"She had a temperature, she looked grey, she was cold, and she had pain in her chest," remembered Jane.
"We found out later that they couldn't record her blood pressure because it was so low. All of those symptoms were a red flag for sepsis."
Bethan was assessed and given a National Early Warning Score (NEWS), which looks at things like blood pressure, heart rate and breathing rate.
Anything above seven indicates a severe risk of sepsis, where care should be urgently escalated to an emergency medical review in an acute care setting.
Bethan's NEWS score was eight - but the paramedic did not recognise that Bethan may have sepsis.
He called for an ambulance but Bethan was not classed as a priority and he did not forewarn the hospital - so when they arrived at almost 20:00 GMT, there was not a resuscitation bed waiting for her.
"A&E that night was chaos, there was no-one taking overall care of Bethan," recalled Jane.
"She was so unwell, her blood pressure was so low, her lips were going blue, she was all blotchy, she was breathing really fast to try and get air in.
"The nurse that triaged her should have known that it was sepsis with a NEWS score of eight."
Almost an hour after being admitted, Bethan was transferred to the resuscitation unit where tests confirmed she had sepsis and she was given antibiotics. But it was too late.
"The doctor said to Bethan 'we think you've got sepsis'," said Jane.
"That's the last thing she heard. They asked me to leave. She had a cardiac arrest about five minutes later and died at 22:00."
Steve frantically travelled back from Dublin, but didn't make it. He was told Bethan had died while driving home to south Wales from Heathrow airport on the M4.
 Steve James
Steve JamesThe Welsh Ambulance Service apologised for the "errors identified in Bethan's case" and said sepsis training was now mandatory, adding that "meaningful changes" had been implemented.
Cardiff and Vale University Health Board, which runs the University Hospital of Wales, said "sepsis awareness and early recognition are priorities" and it was "continuously reviewing sepsis training to improve consistency and accessibility".
The BBC's Freedom of Information request to all health boards in Wales revealed that where there was mandatory training, it was part of other modules and not standalone sepsis training.
The BBC also found the auditing of training was patchy - and some health boards did not log completion rates at all.
"It's absolutely shocking," said the UK Sepsis Trust's chief medical officer Dr Ron Daniels.
"This is one of the biggest killers we face.
"For hospitals not to ensure that their staff are regularly trained is almost negligent.
"It's letting people die because their staff are not trained, but they also perceive that their organisation doesn't take this condition seriously."

The UK Sepsis Trust wants all clinical hospital staff to have mandatory standalone sepsis awareness training to make sure it is caught as early as possible.
"For every hour we delay giving life-saving treatment, the patient's chance of survival falls," said Dr Daniels.
"In rapidly progressing cases like Bethan's, that's even more time critical."
The BBC's research revealed that Aneurin Bevan University health board in south-east Wales had adopted a scheme enabling staff, patients, families and carers to ask for a second opinion about inpatients whose conditions deteriorate quickly.
The Call for Concern scheme has been partially rolled out in three other Welsh health boards, while the remaining three intend to do so in the future. But outpatient areas like A&E units are not included.
In England, there is a way for families to seek an urgent second opinion about patients - including those in A&E - after the rolling out of Martha's Rule, named after 13-year-old Martha Mills, who died in 2021 following missed opportunities to treat sepsis.
Bethan's parents and the UK Sepsis Trust have called for Martha's Rule or similar in Wales - covering A&E departments too.
The National Institute for Health and Care Excellence (NICE) advises that ambulance services should be able to give antibiotics in sepsis cases where combined transfer and handover times to hospital emergency departments are greater than one hour.
The BBC asked every ambulance trust in the UK if they followed these guidelines - only Scotland and the Isle of Wight said that they did. One other, South Central in southern England, has partially implemented it.
The UK Sepsis Trust is urging other ambulance services to follow Scotland and the Isle of Wight's lead - and the NICE guidelines.
Dr Daniels said he would argue "pretty much every" ambulance service's transit times are more than an hour so "we should be giving pre-hospital antibiotics".
"If we lived in the Isle Of Wight, Bethan would be alive," said Steve. "That postcode lottery is just so unfair."
 Steve James
Steve JamesJane added: "I think the worst thing is that I know she could have survived if she had the right treatment.
"I don't want any other family to go through this - because she should still be here with us.
"We want changes to be made - and I feel like Bethan's on my shoulder, saying this is what we need to do."
The Welsh Ambulance Service said it would welcome further research into the benefits of pre-hospital antibiotic administration by ambulance staff.
Steve and Jane want the Welsh government to ensure all Welsh health boards bring in standalone, audited sepsis awareness training.
The Welsh government said sepsis would be a "focus for NHS Wales improvement plans in 2026-27 to ensure consistent, high-quality care".
"We are taking significant steps to improve how NHS organisations recognise and respond to sepsis, including the use of National Early Warning Scores, new safety information for patients and families, and rolling out Call4Concern in all inpatient wards," a government spokesperson added.