Game-changing cancer test means I met my granddaughter
When Pat Grant found out her first grandchild was on the way, her cancer diagnosis made her think: "I am never going to meet this child."
The 78-year-old had always lived life to the full, and been keenly involved in aqua-aerobics and dance classes since her retirement as a social worker.
But when she was diagnosed with inoperable lung cancer, she started losing weight and getting weaker.
After taking part in a Welsh trial of a cutting-edge blood test for cancer, Pat was told her type of cancer might respond well to specific medication.
 Family photo
Family photo"I couldn't get excited about it [the news of the baby] because of how I felt," Pat, from Cardiff, said.
But after signing up for the test, she says she thought: "What have I got to lose?
"They said it's not guaranteed and it's certainly not a miracle cure... it's a gamble in a way.
"Then gradually, gradually I could feel myself getting stronger, almost from my toes up.
"And I've been able to be a grandmother."
She not only got to meet the child, but celebrate her first birthday.
"I'm known as 'Noisy Nanna'. I sit her on my lap and sing the noisy songs with her and she's dancing around... she's got a super personality and is a lovely little thing," she said.
"It's a wonderful honour to think I've been allowed to have that time with her and hopefully a bit more."
 Family photo
Family photoThe Welsh QuicDNA is being rolled out as a standard diagnostic method across NHS Wales for people with later stage lung cancer.
And with extra funding including from the Welsh and UK governments - the roll-out is being accelerated and expanded for people with other cancer types such as colorectal, prostate and cancers which have spread from an uncertain origin.
Further follow-up tests are also being offered to people with lung cancer to determine how well their treatments might be working.
 Maxwell Family Fund
Maxwell Family FundShortly before Craig Maxwell's 40th birthday, doctors found a tumour in his lung - but struggled to get a sample.
It took almost three months for Craig, from Penarth, to find out he had inoperable stage 4 non-smoking lung and bone cancer.
"Those 78 days were the darkest and hardest times me, my family and my closest friends have experienced because you just don't know what your future is going to hold," he said.
"You're not on treatment and just waiting while you are getting ill more quickly.
"Not being able to support my children through that process was completely unacceptable - and something I wanted to change to help other families."
It was then Craig, a former commercial director of rugby for the Six Nations and Welsh Rugby Union, learnt about the QuicDNA project.
Some money had already been raised, but a further £300,000 was needed to get it off the ground.
Since then Craig raised a total of £1.7m to support the research and other initiatives.
He said: "I was able to climb mount Toubkal [in Morocco], all 4,200 metres, I was able to walk the coastal path of Wales within 26 days.
"I was able to take my daughter to the Dance World Cup in Ireland and was able to coach my son's rugby team.
"So having that precision medicine and understanding of my tumour has been an absolute game-changer for patients like me.
"But I'm a very small part of an amazing team."
 Maxwell Family Fund
Maxwell Family FundHow does the cancer blood test work?
Usually doctors try to find out more about someone's cancer by surgically extracting cells directly from a tumour in the body.
But these biopsies can be very invasive and sometimes cause harm, and doctors may struggle to get a sample.
But as cancer cells grow and multiply they shed tiny fragments of their DNA into the bloodstream.
The "liquid biopsy" is a simple blood test that looks for these.
Samples are then analysed in powerful computerised DNA sequencers, some of which cost about £1m each, to build a picture of the cancer's genetic code - which can help determine the best course of treatment.
The test can also be used to monitor how well treatment is working or whether changes in a tumours DNA indicate it is becoming resistant to any treatment.
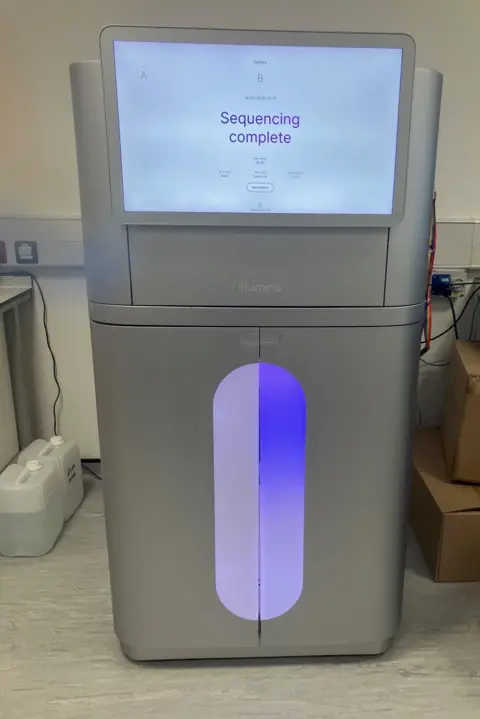
"These DNA blood tests can give you an answer very quickly - within two weeks you can have a genetic reading," said Dr Magda Meissner, an oncologist who is the chief investigator of the QuicDNA study.
"Because patients with advanced lung cancer can deteriorate very quickly if they have to wait many weeks for diagnosis - they might by that time be too unwell to receive the treatment.
"So actually you can save someone's life - they might die six, seven years [after a diagnosis] but could have died within a few weeks if the test had not been done."
But experts warn, more generally, huge challenges remain.
Waiting times targets set by the Welsh government are not being met and survival rates in Wales and across the UK lag behind many developed countries.
"It's incredibly positive news and hopefully we can see a step change in in the way that cancer is diagnosed, because this is the future," said Lowri Griffiths of Tenovus Cancer Care, who is also Chair of the Wales Cancer Alliance.
"But we're still really struggling in terms of our cancer performance times... and what we need to see is investment in whole scale change within the system.
"Unfortunately, some of the international comparisons show that we're really struggling, that we've got a lot of work to do to catch up with the best."