Funding shortfalls delay discharges - care boss
 BBC
BBCA shortfall in government funding is preventing care homes from taking on the number of patients needed to ease pressure on hospital beds, the co-owner of a home in North Yorkshire has said.
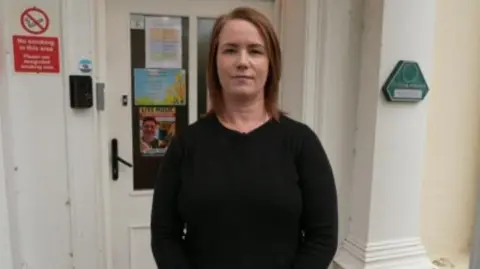
Helen Thompson, from Ochre Care, which runs two private homes in the county, said current funding levels did not match the costs of support needed for many residents coming out of hospital.
Thompson said while her company "absolutely" had capacity, funding from government was "not appropriate to the level of need".
The Department of Health and Social Care said it was tackling the situation with a promise to boost funding by about £4.6bn by 2028-29.
The latest figures suggested that about one in eight hospital beds across the UK were occupied by people who did not necessarily need to be there, with many of those "delayed discharge" patients being older and needing more support.
'Constant juggle'
Thompson, who co-owns the Abbey Lea and Westwood care homes in Selby, which provide accommodation for 39 residents across both sites, said elderly people waiting to be discharged from hospital often had complex needs requiring more support.
"They may need help changing, dressing, eating their meals - and that's all one-to-one care provided sometimes by two members of staff," she said.
As well as the shortfall, Thompson said it could often take "several months" for the appropriate paperwork to be processed and for the funding from the council to be received.
"That obviously affects our cash flow very much, so it's a constant juggle to try and just keep things going smoothly, " she said.
"We absolutely have capacity to take people in, but there can be so many hold-ups and things that prevent you from doing it in a timely way."

Thompson said wider underfunding in social care had left small providers relying on higher fees from self‑funding residents in order to cover the shortfall in local authority payments.
She said that as a provider, the company received about £994 a week for each council-funded resident, but the real cost of providing care was up to £1,300 a week.
"About 65% of our residents are not funded to the amount they need to be appropriate to their dependency, so with that, it's the privately-funded residents that subsidise the gap.
"So we have to be sure that we have the right mix of both."
Thompson called on the the government to better support smaller care providers.
"I'd say to the government: fund social care appropriately because people deserve quality of care towards the end of their life," she said.
"If we disappear then it will cost everyone a lot more because we provide great, high quality care at a lower cost to a lot of the bigger groups."
'Sustainable funding'
Wendy Taylor, chair of the Local Government Association's health and wellbeing committee, said the system "remains in desperate need of sustainable funding".
"If we are to be able to ensure that everyone who draws on care and support can live the dignified and independent lives they want to lead, we need a financially sustainable system rooted in prevention and personalised care," Taylor said.
"Care providers are under increasing pressure from rising costs, inflation and changes to employer National Insurance contributions.
"Councils, as commissioners of social care, work closely with providers to ensure the best possible provision of services for local people, but until the sector is adequately funded, the consequences of a lack of resources and a system that is under strain will remain."
 Getty Images
Getty ImagesThe Department of Health and Social Care spokesperson said the current government had "inherited a social care system facing significant challenges".
"But we are turning it around by making available a funding boost of around £4.6bn by 2028-29 and launching the first ever fair pay agreement to boost recruitment and retention of care workers," they said.
"We are also creating a National Care Service, based on higher quality of care, greater choice and control, and joined-up neighbourhood services."
Richard Webb, North Yorkshire Council's corporate director for health and adult services, said adult social care was facing significant pressures nationally.
"We cover England's largest county and are responsible for delivering and commissioning social care across vast rural areas, market towns and villages, Webb said.
"Each hour of social care in our rural communities can cost £5 more than in other parts of the country because of the travel costs and the longer journey times between people - a single home care round can cover a geography larger than the size of London.
"That's why we welcome the national commission, led by Baroness Louise Casey, which is looking at how social care should be delivered and funded in the future."
Listen to highlights from North Yorkshire on BBC Sounds, catch up with the latest episode of Look North.