Call centre and robot helping 'one-stop' GP cut waiting times
 BBC
BBCStaff at the Riverside Surgery in Brigg, North Lincolnshire, describe it as a "one-stop shop" for patients. The BBC spent a morning there to see how its call‑handling centre and new dispensing technology – including a robot helper and 24-hour prescription vending machine – are helping to cut waiting times and manage demand.
On a typical January morning, the Riverside Surgery feels unusually calm for a practice serving 24,000 patients across five sites.
Many of us have come to dread the 8am rush to secure a GP appointment, but things are done very differently here.
Even by 9am, the downstairs waiting room is quiet. Upstairs, the real work is well under way.
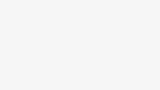
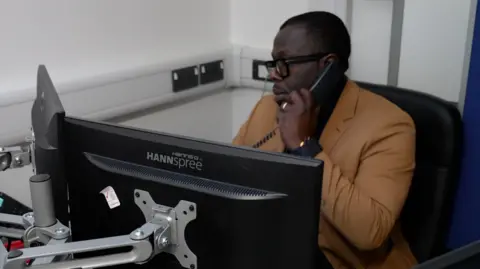
Behind an unmarked door is the "Patient Room" – the on-site call centre where "care navigators", nurse practitioners and a GP triage every request for help – before face‑to‑face appointments are made.
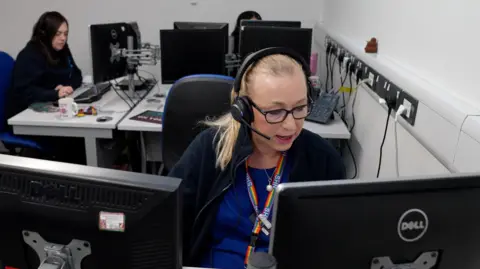
Dr Chinenye Ekpeh, a GP partner, is on duty.
"I call this the engine room of the practice," he says. "Virtually every person who calls in will be spoken to by a clinician."
For patients expecting to call up and talk to a receptionist, it might be a surprise, but the model is designed around clinical decision‑making from the first moment.
"It's about knowing who needs to be seen immediately, who needs to be seen today and minimising risks," Ekpeh says. "If someone needs to come in, we bring them in."
This new way of working also involves an online system: patients fill out a digital form before talking to someone on the phone.
The idea is to handle cases more efficiently and ensure GPs see those who most need them.
One of the first voices callers hear is Julie Johns, the care navigation lead.
"The volume of calls is huge," she says. "We've got a very large older population.
"The system now is working great – patients are being seen much quicker."
While urgent cases are seen the same day, Johns says the changes have also helped reduce waiting times for advance appointments.
"People expected to be seen in a few days, but had to wait weeks. Now the longest wait is about a week."
Those who struggle to fill out the online forms are helped by the team, while patients with no internet access can talk on the phone.
Hayley Mason, a care navigator, is trained to help direct patients to the right colleague.
"If someone's unsure about the online form, we stay on the phone with them. If photos are needed, we walk them through it. That really helps a lot of elderly people," she says.
"It's never a quiet day, but this is the best the system has been since I started."
While the surgery is at the centre of the operation, much of the work happens well beyond its walls.
At 10:30, I meet Amanda Barlow and her team. She's a registered nurse in the palliative and supportive care team and spends most of her days in the community.
"We go into care homes, we see the housebound, the frail, the elderly and people at end of life," she says.
Barlow covers 13 care homes, visiting most weekly.
"They just can't come in, so we need to get out to them. It certainly hasn't always been this way, but it's definitely the way forward."

Riverside operates as a small health hub, providing minor surgery, dentistry and 24‑hour prescription collection.
By 11:00, the waiting room, optician's and adjacent pharmacy are much busier, with a steady stream of people arriving for appointments or to pick up medication.
And there is a problem for Michelle Slimm, the business manager, to overcome: one of the GPs has called in sick.
It's something the call centre can handle, insists Slimm, who is confident that all the patients who need to be seen will be.
"We're a modern general practice," she says. "We've got a theatre for minor surgery – hand surgery, eye surgery, vasectomies, plastic surgery – plus a dentist and a pharmacy.
"It's very much a one‑stop shop. Rather than everyone seeing a GP first, we direct people to the right service."
Robot helper
Technology plays a big part in helping to modernise services, says communications lead Ben Watson.
He shows me "Vincent", a dispensing robot used to deliver medication.
Vincent is a bit like a vending machine, selecting tablets from shelves by barcode, before sending them down a series of chutes to the pharmacy.
Outside is a 24‑hour prescription dispenser, called PharmaSelf24, which allows patients to pick up medication using a secure code.
"It frees up staff and avoids queues," Slimm explains.

By 12:00, Chris Darlington, a volunteer from the patient participation group, has dropped by.
He has watched the changes being brought in and tries to see things from a patient's perspective.
According to Chris, some people initially struggled with the modernisation, but many now see the benefits.
"People know that if they have a problem filling something out, they can come in and someone will help them," he tells me.
The 24-hour dispenser has helped tackle prescription waiting times – a key concern.
"You get a message, put a code in a box, and there it is, 24 hours a day," he adds.

It is the end of a pretty busy morning and GP Dr Manish Khandelwal is about to take his break.
He tells me that the new triage model is making a big difference by reducing unnecessary face‑to‑face appointments, cancellations and no-shows.
"Some appointments didn't need a doctor in person," he says. "Those could be used for someone else.
"The key feedback comes from patients. If it's working for them, it's working for us."
At 1pm, it is time to leave. Across its five sites, Riverside insists it is trying to balance clinical safety, patient expectations and the realities of modern general practice, while encouraging people to adapt to new ways of accessing care.
The transformation, via the "engine room" and the technology surrounding it, appears to be well under way.
The challenge now, Slimm says, is helping patients adjust to the new realities of primary care – while ensuring GP practices can continue to deliver for the communities that rely on them.
Listen to highlights fromLincolnshire on BBC Sounds, watch thelatest episode of Look Northor tell us about a story you think we should be covering here.
Download the BBC News app from the App Store for iPhone and iPad or Google Play for Android devices