'Patients get care they need, not what they want'
 Josh McLaughlin/BBC
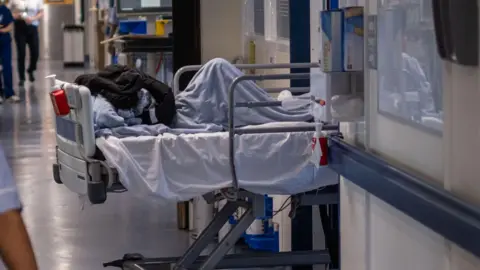
Josh McLaughlin/BBCIt is 08:30 GMT and a dozen patients who have been queuing outside on a gloomy January morning stream into Princes Park Health Centre in Eastbourne.
At the same time, 30 patient calls immediately queue up on the phone lines and medical forms filled in by patients online begin appearing on the system.
It is the start of a busy morning. More than 150 patients request care in person, by phone or online before midday.
The health centre has been a pioneer in piloting the NHS "total triage" system over the past 14 months, in which patient requests are screened and assessed by a dedicated GP before an appointment is booked instead of a "first come, first served" early morning race.
 Josh McLaughlin/BBC
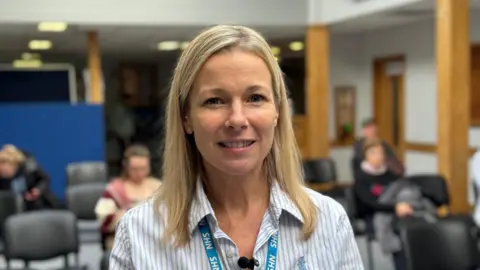
Josh McLaughlin/BBCSteph Williams, managing partner and director of Eastbourne Healthcare Partnership, says it has been a "game-changer" for patients and staff.
The health centre used to receive more than 350 calls each day but now receives less than half that amount.
Williams said: "It means patients are seen by the right clinician at the right time. Patients receive what they need, not necessarily what they want."
A follow up text message, email or call lets patients know if they have a face-to-face or telephone appointment, or tells them to seek help from their pharmacy, NHS 111 or A&E.
Online requests for routine appointments, sick notes, prescription requests, test results and referral updates can also be made 24 hours a day.
Lead receptionist Sheri said: "We look at the urgency of the situation and make sure each patient is getting given the best care, whether that's with us or signposting to an another appropriate service."
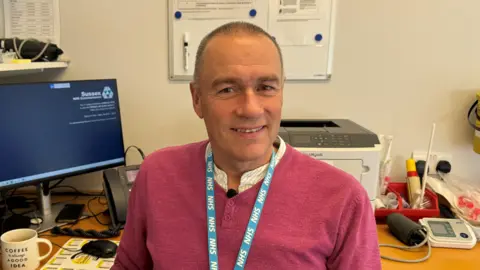
Senior partner Dr Jonathan Andrews said: "There's a limit to the capacity of the practice.
"Our reception staff get a lot of the backlash, criticism, anxiety and abuse from the patients sometimes."
On an average day the practice has seven GPs offering a total of around 180 face-to-face and telephone appointments, as well as a paramedic practitioner, a first contact practitioner, six nurses and two phlebotomists taking blood tests.
 Josh McLaughlin/BBC
Josh McLaughlin/BBCAndrews said a peak in flu-like symptoms had seen a peak in demand this January, meaning some GPs were taking admin work home in the evenings after seeing patients all day which was "not good for them".
He said better funding of primary care would mean they could expand their services to deal with more patients.
"If we see patients we can stop them going to A&E and then there'll be a smoother process through A&E, not so many people will be admitted to hospital and the whole system would run a lot more smoothly," he said.
On 14 January, East Sussex Healthcare NHS Trust declared a business continuity incident for two days at Eastbourne District General Hospital in light of extreme and sustained operational pressures both in its emergency departments and across the wards.
The Department of Health has been contacted for comment.
Follow BBC Sussex on Facebook, X, and Instagram. Send your story ideas to southeasttoday@bbc.co.uk, or WhatsApp us on 08081 002250.