'The NHS is at risk – here's how we save it'
 JAMIE NIBLOCK/BBC
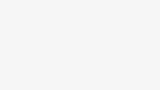
JAMIE NIBLOCK/BBCA National Health Service that acts as a safety net for the most vulnerable is under threat, according to recently retired hospital boss Nick Hulme.
After four decades in healthcare, he says it is time to be honest about what the NHS can deliver – before it is lost forever.
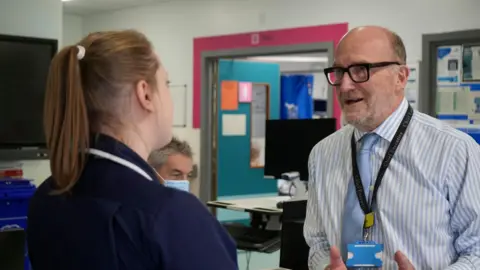
Mr Hulme began his career as a porter in A&E, moved into management in sexual health services and later led Ipswich and Colchester hospitals as chief executive of East Suffolk and North Essex NHS Foundation Trust.
He was also a troubleshooter for NHS England and was appointed a CBE for services to healthcare.
As he steps down, he says the NHS is facing one of its most difficult periods in decades.
Here are the changes he believes are vital to secure its future.
Be honest about what the NHS can deliver
 JAMIE NIBLOCK/BBC
JAMIE NIBLOCK/BBC"We've heard time and time again: the NHS needs more money or more staff or it won't survive," he says.
"But there hasn't been an alternative pushed – either politically or by the public – for how the NHS really needs to change."
Mr Hulme says the mood has shifted. "We now have politicians who are actively calling for the end of the NHS," he warns.
Colchester Hospital, which he managed, serves patients from areas around Clacton-on-Sea, including Jaywick, officially ranked the most deprived neighbourhood in England and illustrating the safety-net role the NHS plays in coastal Essex.
Mr Hulme has met Reform UK leader Nigel Farage, Clacton's MP.
"Nigel Farage is very clear that he doesn't believe the NHS is the right system for this country and favours a more insurance-based approach to healthcare," says Mr Hulme.
 PA
PAHe strongly disagrees, arguing an insurance-based health system would weaken protection for the poorest.
"I don't think that is the right answer. It doesn't provide the safety net for the most vulnerable."
That protection, Mr Hulme argues, must remain the NHS's core focus, and cites the United States as a warning.
"Millions of people without health insurance have very poor lives," he says.
Mr Hulme believes outcomes and access are closely linked to income, and insurance gaps can worsen inequality.
Farage said in 2024 the UK should "re-examine" how the NHS is funded, while also supporting the principle of free care at the point of delivery.
In response to Mr Hulme's comments, Reform UK said: "Reform UK and Nigel Farage have always said that we will never privatise the NHS, nor will we ever charge people to use it."
Make NHS investment count
 RICHARD KNIGHTS/BBC
RICHARD KNIGHTS/BBCMr Hulme acknowledges recent investment in NHS staff and buildings but says it has not consistently led to shorter waits or better cancer outcomes.
Two studies led by University College London found UK patients received chemotherapy and radiotherapy less often than in comparable countries and faced longer waits, helping explain why survival lags internationally.
Separate analysis shows the UK trailing Scandinavia on several common cancers.
"It is difficult to effect change in what is effectively a state-funded monopoly," says Mr Hulme.
Despite the challenges, he remains a passionate advocate of the NHS.
"It is without doubt the best healthcare system in the world – though not always delivering the best healthcare. That's the challenge."
He warns that if more people turn to private care, NHS investment could suffer, and that if productivity does not improve, critics will seize on it.
"At the moment, I think there's a danger we're providing ammunition for their argument. The challenge is on the NHS."
From hospitals to homes – focus on prevention
 NIKKI FOX/BBC
NIKKI FOX/BBCFor Mr Hulme, the core challenge is healthy life expectancy, not just life expectancy.
Hospitals are seeing rising numbers of frail, older patients with conditions such as COPD, type 2 diabetes, and obesity‑related cancers - what Mr Hulme calls "diseases of poverty and deprivation".
He believes the safest place is often not hospital if someone does not need to be there.
Unnecessary hospital stays can lead to physical and psychological deconditioning and isolation from family.
But prevention takes time. Mr Hulme says that is one reason governments hesitate to invest in the NHS. "We don't see the return quickly enough in the political cycle for ministers to take the credit," he says.
Embrace AI to improve care
Mr Hulme says the NHS workforce must change radically – and fast.
"Thousands of jobs that exist today simply won't exist in a few years. We need to stop training people for roles that won't be there," he says.
At Colchester Hospital, barcode automation replaced minutes of hand-writing blood test labels.
In screening, AI is already showing promise: UK trials of the Mia tool detected 12–13% more cancers without increasing unnecessary recalls and modelled workload reductions for radiologists.
 Getty Images
Getty ImagesThe UK National Screening Committee insists any AI rollout must be evidence-based, a principle that Mr Hulme supports. The question, he argues, is how to use the time saved.
"Do we spend those extra minutes talking to patients or seeing more people to improve productivity?"
He describes today's reality as "21st-Century healthcare delivered with 1960s processes" and says the NHS should catch up with sectors such as banking, where digital self-service is routine.
Support, he notes, will still be needed for those who struggle online.
"We don't have the burning platform of competition, but we do have the burning platform of affordability," he says.
"The NHS will be under threat unless we radically change how we deliver care."
Let doctors focus on complex cases
 Reuters
ReutersMr Hulme argues not all care needs to be delivered by a doctor or surgeon.
Some tasks, he says, can be done safely by other professionals under supervision. He cites sexual health services, now largely nurse-led, freeing doctors to focus on complex cases.
"We need to have a conversation with the professions about working in silos and whether we need all the qualifications," he says.
He acknowledges pushback over physician associates and anaesthetic associates.
The British Medical Association – the doctors' professional body – has raised concerns about patient safety and role clarity and pressed for clearer regulation.
A government-commissioned review by Gillian Leng backed up a number of these concerns when it reported in 2025.
Mr Hulme's position? Define roles clearly, supervise properly, and let doctors concentrate on work only they can do.
On intense competition for speciality training, he says supply and demand may mean some doctors will need to rethink career plans.
Asked what he would say to politicians who claim the NHS cannot be fixed, he replies:
"If you cut me, I'd bleed blue. I love the NHS – it's the most precious thing about living in this country.
"It's so special we can't afford to lose it. We can fix it, but we have to look at international best practice – and it's down to us."
The government's response
A Department of Health and Social Care spokesperson said: "Under this government, the NHS will always remain a publicly funded service free at the point of use.
"But it does need fundamental change, and through modernisation and record investment, we've cut waiting lists by more than 200,000 and boosted productivity so patients get seen quicker and taxpayers get maximum value for money.
"There's a long way to go, but the NHS is on the road to recovery, and our 10 Year Health Plan will create an NHS fit for the future."
Follow East of England news on X, Instagram and Facebook: BBC Beds, Herts & Bucks, BBC Cambridgeshire, BBC Essex, BBC Norfolk, BBC Northamptonshire or BBC Suffolk.