Can Scotland learn from Ireland’s health service?
The NHS in Scotland is looking for radical solutions to its problems so can it learn any lessons from its neighbour, Ireland?
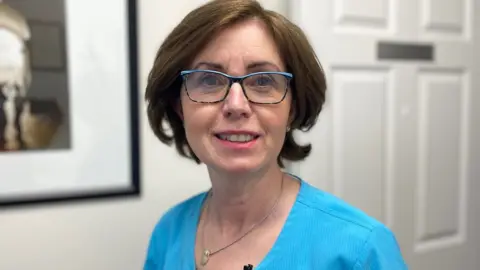
When Anne-Marie Davy's doctors found a large mass in her abdomen in 2015 they suspected it was cancer and said she urgently needed another scan.
In Ireland's public health service, she was faced with a choice.
She could wait several weeks or even months in the public health system or she could go private and be seen in days.
"You want to get it dealt with right away, because every day matters," says Anne-Marie, who is from Edinburgh but lives in Galway.
"I didn't have health insurance but I had to find the money to go private, because I was told I was an urgent case,"
Anne-Marie was fast-tracked by paying for private tests, which found a rare cancer in her appendix.
She then went back into the public service for complex surgery in Dublin.
The two-tier health system that operates in the Republic of Ireland ensured she was diagnosed quickly and then offered highly specialised treatment - boosting her survival chances.
But she feels guilty about how the system works.
"It's wrong that it's a form of queue-jumping," Anne-Marie says.
"If you're in the public system you have to wait so long before you can be seen. Sadly some people probably die before they are seen."

Long waits for potentially life-saving diagnostic tests are common in Ireland, as they are in Scotland. The two countries have similar populations but very different health systems.
The Irish Cancer Society estimates that more than 200,000 people were waiting for scans, such as MRIs or ultrasounds, at end of 2022 - with 60% waiting more than three months.
Data from Public Health Scotland shows 114,061 patients were waiting for scans here, with almost 60,000 of them waiting longer than the six-week target.
Healthcare systems everywhere face huge challenges post-pandemic.
In Scotland, this has meant that radical solutions, which would breach the founding principles of a universally free NHS, appear to be up for debate.
In November, health board minutes seen by the BBC showed that officials had discussed the idea of asking wealthier patients in Scotland to pay for some health services.
Scotland's Health Secretary Humza Yousaf - currently an SNP leadership candidate - said he would never consider charging anyone for NHS treatment.
But in a poll for BBC Scotland, more than one in five respondents said they or a family member had paid for private medical care in the past 12 months.
And those who work in Ireland's private hospitals say the two-tier system there works for hundreds of thousands of patients every year, who get exceptional service.
"At the end of the day, Mary or John really has no desire to know whether the hospital they're being treated in is public, private, or voluntary," says Jim Daly of the Private Hospitals Association.
"All they want is to get the best level of care."
Ireland's state health system is unique in Europe because it doesn't cover the whole population.
Around 45% of people have private health insurance which allows them to get faster access to care.
Thousands of other patients get access to private hospital treatment paid for by the National Treatment Purchase Fund, a government initiative aimed at reducing public hospital waiting lists.
In primary care, only about 40% of people have free access to a GP and others, who aren't insured, have to pay full prices.
So the system is complicated, even within individual GP surgeries.
In Kilcullen, just outside Dublin, Pamela Tracey pays 60 euros for her doctor's appointment because she isn't insured.
"It's fine if you're going now and again but it adds up pretty quickly. It's a lot of money in the current climate."
Special medical or GP cards, which provide free care, are reserved for those on the lowest incomes, those with long-term illnesses, young children, and elderly patients.
Older people also get regular checks but others with chronic conditions like diabetes can face difficult choices about receiving proper medical care.
Kilcullen GP Dr Deirdre Collins says she factors this into every discussion.
"If you come in today and you've got pain in your chest, and I want to think about whether you've got cardiac ischaemia, if you have private healthcare, you can be seen in a private setting maybe today, maybe tomorrow, depending on how urgent I feel it is," Dr Collins says.
"If I want to do that in a public setting, I probably have to send you to Casualty. That's not a way to be, at all."
Prof Steve Thomas of Trinity College, Dublin, says this kind of urgent care is where the two-tier system doesn't work.
"The problem is that if you're not that well off, you don't qualify for free care, but you can't afford insurance, then you're caught in a trap whereby you can't really afford to pay 60 euro to go and see your GP.
"And then your problems get worse, and maybe you end up going to the emergency department and clogging that up, which is really when the system breaks down completely."
Politicians in Ireland agree that the situation there needs improvement. And unlike in Scotland, there is broad consensus on the direction of travel.
Sláintecare, a programme of reform supported by all political parties, aims to transform healthcare towards delivering universal equal access to services for every citizen based on need, and not ability to pay.
"I think there's been a realisation that the system has become quite fragmented, it's become very unequal and unfair and that's quite expensive too," says Prof Thomas.
"Alongside that, there's a realisation that if your health system doesn't work, your economy doesn't work. So I think it's redoubled efforts to invest more."
Charges of 80 euro a night for public hospital stays are due to be abolished this month, after a campaign by the Irish Cancer Society.

"We're all going to be patients at some point in our lives," says Rachel Morrogh from the society. "We need to resource public health care so it's equipped to deal with that."
But she says there are fears that well-meaning policies could create similar problems to those in Scotland.
"There's a concern that if it became completely universal and much more consistent with the NHS model, then you would end up very quickly in a situation where demand would outstrip supply and it wasn't affordable anyway," says Ms Morrogh
Meanwhile, there are growing calls for a more open conversation about the future of Scotland's NHS.
But Prof Thomas says there's no gold standard model for healthcare reform anywhere.
"One of the key challenges is to sort out what works best for Ireland within an Irish context, the budget and the values and the politics," he says.
"And I think that's something that Scotland has to embrace, to work out what's best for you."
