"Dis na death trap for us" - Pipo living wit HIV lament USAID shutdown

- Author, Dorcas Wangira
- Role, Africa Health Correspondent
- Read am in 6 mins
Mike Elvis Tusubira na Ugandan motorcycle taxi rider wey dey live wit HIV since 2022, wen dem first diagnose am.
For am—one of di 1.4 million pipo for Uganda wey dey live wit HIV—USAID na lifeline. Di next three months, e say, na "literally a matter of life and death."
"Di stopping of all USAID projects don affect me psychologically. I no know wetin go come next. Wetin go happun to me?" e tok.
"My counsellor tell me say e no longer dey di clinic. Wetin go happen to my pikin and partner?"
"I dey worried about my future. And actually, di future fit no dey dia. Becos no mosquito nets, no ARVs, no condoms, no services at all."
Mike wife dey HIV-negative and she dey rely on PrEP (pre-exposure prophylaxis), a medicine wey dey reduce di risk of contracting HIV.
Since di abrupt shutdown, neither im nor im partner don replenish dia supply of di life-saving medicine. Di uncertainty, e say don already put a strain on dia relationship.
Uganda dey among di top ten recipients of USAID funds in Africa. According to US goment data (ForeignAssistance.gov), di kontri receive $295 million in health funding from di agency in di 2023 financial year—ranking third afta Tanzania ($337 million) and Nigeria ($368 million).
End of Di one wey oda users dey read well well
Uganda health sector dey heavily reliant on donor funding.
USAID support dia HIV/AIDS, malaria, tuberculosis, and leprosy programs. E also dey fund maternal and child health services and emergency health assistance. Foreign donors dey fund 70% of Uganda AIDS response.

Health workers dey affected
Thousands of healthcare workers dey impacted by di USAID funding freeze.
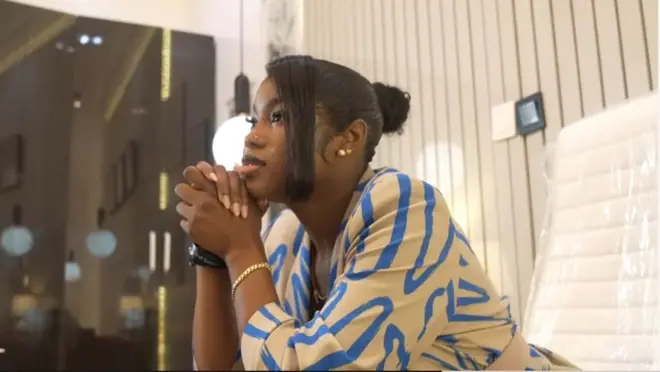
Shamirah na clinician with Reach Out Mbuya (ROM)—a faith-based community organization wey dey provide medical and psychosocial support to pipo living with HIV in Uganda. She bin dey based at Kisenyi Health Centre IV, wey dey serve a densely populated slum in Kampala.
On average, she dey attend to 200 patients wit HIV/AIDS and tuberculosis daily. But after di stop-work order, all ROM-supported health workers bin dey laid off.
Now, di Tuberculosis Unit also dey silent. Di Orphans and Vulnerable Children section— wey also dey funded by USAID—too dey shut.
"We dey wait for di 90 days. So, dis compulsory leave, I no prepare for am," she tok.
"E dey so abrupt, we no get enough time to prepare. We no get a proper handover of evritin for di facility. We just stop working."
Uganda goment respond
Uganda Ministry of Health say dem dey explore ways to integrate essential services into routine healthcare to minimize disruptions.
"As such, contracted staff wey dey willing to continue to work in di spirit of patriotism as volunteers until we harmonize wit di United States, goment dey encouraged to contact di respective hospital directors or my office," na so one official statement from Health Permanent Secretary Dr. Diana Atwine tok.

Panic in Malawi
Further south in Malawi, USAID-funded activities also don stop.
For Macro Mzuzu Clinic, a key provider of HIV services for di kontri northern region, di gates dey shut. Vehicles dey idle. No sign of activity.
According to local resident Eddah Simfukwe Banda, wey dey depend on di clinic for her antiretroviral treatment, di clinic don dey deserted since dem issue di stop-work order.
Even afta di US State Department issue a waiver on 28 January to allow di delivery of medicine such as ARVs, many clinics still remain closed.
Witout di critical staff wey dey coordinate USAID activities, distributing medicines don become a challenge.
Even wia services technically dey permitted to resume, many contracts remain uncertain. Health workers dey unsure of wetin dem fit and fit no do.
Di Trump administration plan to significantly reduce USAID staff by more dan 90%.
Atul Gawande, USAID former Global Health Assistant Administrator, post on X say di agency workforce go dey slashed from 14,000 to 294—wit only 12 staff assigned to Africa.
More dan 30 NGOs also dey severely impacted by di funding freeze.
Malawi receive $154 million from USAID health budget for 2023, wey make dem di 10th largest recipient for Africa.
Di kontri remain one of di poorest and most aid-dependent in di world. According to di World Bank, Malawi dey vulnerable to external shocks—including prolonged droughts, cyclones, and erratic rainfall. Disruption of dis magnitude for dia healthcare system present an ogbonge challenge.
Eddah Simfukwe Banda dey worried about her own fate—and dat of her sister-in-law, wey also dey rely on donor-funded medication.
"As pipo wey dey on ART treatment we get several options to dis case. One we get to pray as Malawians. Dose of us wey believe and depend on God say we get God wey dey open doors wen one dey closed," she tok.
Right to Care, anoda USAID-funded health provider, dey forced to suspend most of dia operations, including dia HIV outreach programs for LGBTQ+ individuals for northern Malawi.
One staff member describe di facility as "semi-deserted," wit only a handful of personnel allowed through a small walk-in gate.
Grim outlook
According to UNAIDS, di global outlook dey grim.
For 2023, e bin get 630,000 AIDS-related deaths worldwide and 1.5 million new infections.
While infection rates don dey decline in di worst-affected kontris, di impact of di USAID shutdown fit reverse dis gains.
"If you take away dis major contribution by di United States goment, we expect say in di next five years, additional 6.3 million AIDS-related deaths go dey," UNAIDS Executive Director Winnie Byanyima tell BBC Africa Daily podcast.
"8.7 million new infections go dey, 3.4 million additional AIDS orphans go dey. I no wan sound like a prophet of doom, but I get a duty to give di facts as we see dem."
One major concern for health experts na drug resistance. According to Médecins Sans Frontières (MSF), any interruption in HIV treatment fit get severe consequences.
"Any interruption to HIV services and treatment dey deeply distressing to pipo wey dey care and emergency wen e comes to HIV treatment," na so Tom Ellman, director of di South Africa Medical Unit at MSF Southern Africa tok.
"HIV medicines gatz dey taken daily or pipo go run di risk of developing resistance or deadly health complications."
Byanyima echo dis concerns, sharing di words of a desperate patient:
"One pesin living wit HIV don describe am as, 'Di na death trap. Please tok to di American goment. Dis na death trap for us. If I no get my tablets next month and di following month, how much longer I get to live?'"
Africa fit fill di gap?
For decades, di US na im be Africa most significant public health partner.
Since di launch for 2003, di US President's Emergency Plan for AIDS Relief (PEPFAR) don save more dan 25 million lives.
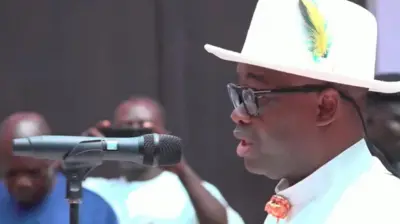
"In di past year, USAID give $8 billion of aid assistance to Africa. Seventy-three percent go to healthcare," Africa CDC Director General Jean Kaseya tell di BBC Newsday program on 29 January.
Health experts warn say replacing dis funding go dey extremely difficult.
African goments don make strides in reducing aid dependency. Kenya now dey fund nearly 60% of dia HIV response. South Africa dey cova almost 80%.
But for many low-income nations, debt burdens, climate disasters, and economic shocks dey make self-sufficiency nearly impossible.
Amref Health Africa CEO, Dr. Githinji Gitahi, warn say witout urgent action, global health security dey at risk.
"Dis go require African goments and Africa CDC to increase dia own funding, wey dey almost impossible under di current debt distress conditions," e tok.
"With accelerating outbreaks from climate change and human-environmental 'conflict,' dis go leave di world fragile and unsafe—not only for Africa but for evribodi.”