BBC Innovators: Africa 'game changer' inside fight against malaria
- Author, Alfonso Daniels
- Role, Kitgum, Uganda
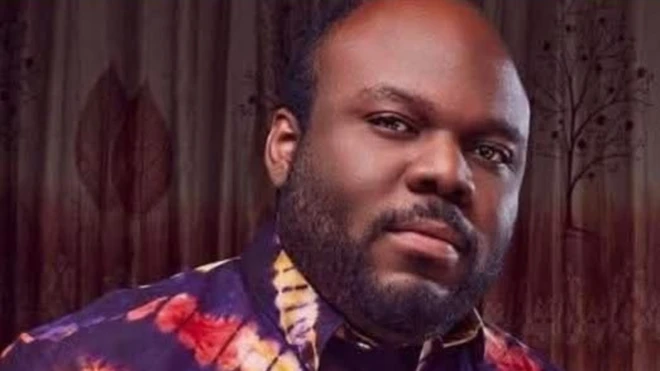
"At first dis project start like game, we bin just be friends wey come togeda to do sometin wey dey sweet belle," na wetin 26-year-old Brian Gitta tok.
"But afta about one year I say, come guys, we dey enjoy oursef, but I think say we fit change lives wit wetin we dey do."
Brian dey tok to di BBC just weeks before im win di Royal Academy of Engineering Africa innovation prize on top im malaria testing tool.
Four years before now, Brian and im fellow students for Makerere University, come up wit dis chickini moni tool wey pesin fit use again, dem call am Matibabu wey dey check and find malaria sharp sharp without to remove blood from pesin bodi.
Although e still dey sample stage, di society judges callhis malaria testing machine "simply one game changer" for di fight against dis disease wey dey kill.
Magnets and matiscope
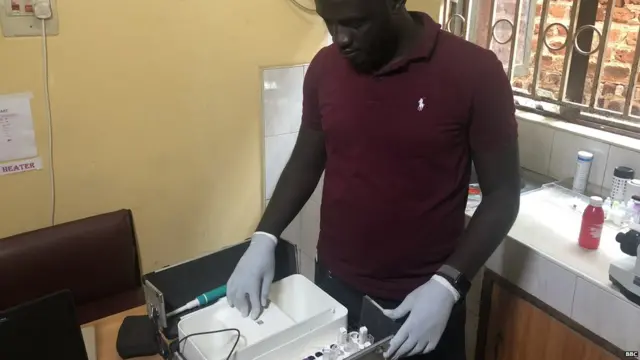
'Matibabu' wey mean "treatment" for Swahili, dey uses magnets and one small special design portable tool dem call matiscope.
Di device dey shine red light show for di finger of pesin wey use am, dey find wetin dem call hemozoin crystals, wey be product from malaria parasite.
Those wey make am believe say Matibabu fin change ot even turn di situation on to say e go make testing time dey fast since e no need to remove blood, and also e no dey use use injection needles wey pikin especially dey struggle wit.
End of Di one wey oda users dey read well well

Last year, 9.5 million pipo for Uganda suffer malaria including 5,100 wey die inside, most of dem na pikin dem be.
"My pikin bin suffer convulsions without any sign and e no gree eat, im bin happy dey play around one moment and dey go school, and e fall sick di next," Achan Nighty tok as she sidon on top di bed near her six-year-old son for Kitgum Hospital inside northern Uganda.
"We dey live very far from di clinic inside one small farm. I need to take care of my three oda small pikin dem and I no get moni, so it take me three days to come here. I pray say e neva dey not too late." she tok.

Brian first come up wit dis idea wen im suffer one serious malaria sickness, join wit typhoid.
Wen e dey hospital, e bin imagine na quick and pain-free testing machine dem go use check am without needles and even choom im bodi.
Im join wit graduates wey get skills for engineering, computer sciences and infectious diseases.


Di BBC Innovators story dey show how pipo wey get beta ideas dey solve problems for many parts of South Asia and Africa
Learn more about BBC Innovators.
Di latest number five-generation Matibabu model only need two minutes to find malaria as against 30 or more minutes wen e go take wit di use of microscope.
Di oda testing method wey dem accept now, na Rapid Diagnostic Tests, wy dey take up to 15 minutes and e require to remove blood but e no fit show di number of parasites wey fit lead to too much tresatment.
Since Matibabu no require any blood sample, e n need specialist wey get medical training to operate am, so na sumtin di communities demsef fit use on dia own.
Lack of resources
Even sef Matibabu dey connected to smartphone, meaning say e fit collect data, send alert go give health teams informate about malaria sickness wey e find.
"Many pipo dey live for village and di roads dey bad, so to go health centre na problem," according to Kitgum hospital director Dr Geoffrey Akena.
"To try to solve dis problem we don send village health teams wey dey travel around di region dey treat pipo, but we no get informate so dem just dey waka upandan not knowing where dem need to face."

For many parts of Uganda, e reach 1.5 million bad case dem geton top malaria wey dey happun evri year wey dey turn to serious complications, according to di Ministry of Health.
E mean say dis disease don dey too late to treat. Malaria dem fit cure am sharperly and e go show improvement if treatment happun within di first 24 hours.
Matibabu go help close dis gap and ensure say treatment dey readi and available for those wey need am quick-quick.
Game changer?
But no be evritin dey clear. Di current Matibabu machine fit check and find 80% of malaria cases, e still far from 99% wey be di level international practice accept, na sometin Brian dey aware of.
"Our machine heavy pass di previous model dem, e dey connected to one personal computer, and you no fit put your finger since di light dey shine on one blood sample. But our focus now na on di next lab test dem wit 300 patients and to perfect di machine, we go improve di design later."
Brian dey tok while im dey hold im machine wey dey like small suitcase-size, dey stand outside one clinic outside of Kampala, wey be one of many clinic dem im visits to explain to doctors how im machine dey work.
Upon di challenge dem, Brian still dey confident say Matibabu go work and im dey look for $600,000 so dem fit enta market by di next two years - wit hope say n aim machine dem go use for future to test for oda diseases like anaemia.
Consider say malaria dey kill almost half a million pipo evri single year, mostly small pikin dem wey dey live inside Sub-Saharan Africa, so Brian career and reputation dey at stake.
Dis BBC stori dem make am wit helep moni from Bill & Melinda Gates Foundation