Thank you for joining uspublished at 18:59 GMT 22 January
Thank you for joining us as we have spent the day showcasing the pressures the NHS is under, and how it is coping.
Here are some of the highlights:
Health Secretary Wes Streeting spent two hours being grilled by local BBC radio stations, many of whom raised issues such as the pressure on staff, waiting list targets, dental care and patients receiving care in corridors, which has been highlighted as an issue across the board.
Streeting says the NHS is broken, but it is not beaten, and that turning it around "will be a marathon".
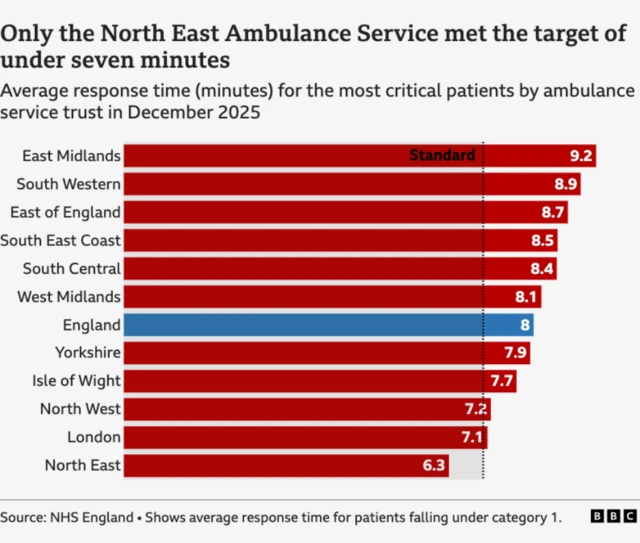
Other talking points throughout the day have included cancer care and waiting list targets; a diagnostic centre in a shopping centre; ambulance response times; 'AI patients' being used to train the next generation of medics; and delayed discharges leading to backlogs.
Elsewhere there have been some positive stories, such as a woman paralysed by cancer who learned to walk again against all the odds, and paramedics have been talking about what a privilege it is to do their jobs.