'NHS is in recovery but not out of the woods'published at 10:25 GMT
Matt Cole
Senior political reporter
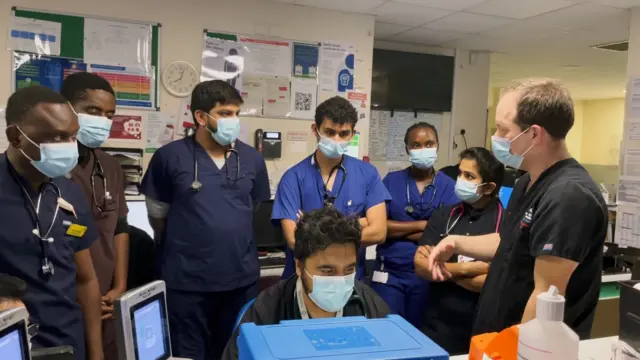
Giving a condition check on the NHS under Labour, Streeting told BBC Radio Cornwall's Julie Skentelbery that the NHS is in recovery but not out of the woods.
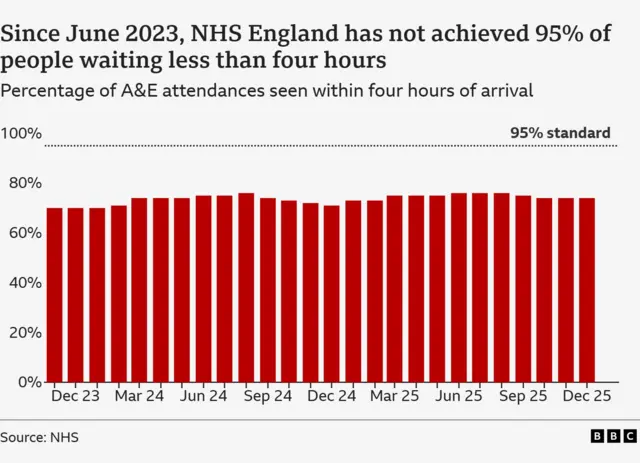
The question for patients though is: is he right when he says there has been "real progress in 18 months" of Labour Government?
Waiting lists are down - but still nowhere near hitting the target for 18-week maximum waits that patients are told they should expect.
 Image source, PA
Image source, PA