This article was last updated in March 2021.
Since the rollout of Covid-19 vaccines across the country began in late 2020, millions of adults have already been vaccinated.
By the beginning of March 2021, three vaccines have been approved for use in the UK - one made by Pfizer/BioNTech, another by Oxford AstraZeneca and a third by Moderna.
Now, the team behind one of the jabs has said they’ll begin trialling the vaccine on children and young people to see how effectively it works on them.
Around 300 children will join the trial of the Oxford AstraZeneca vaccine – but what does that all mean? We asked our Instagram followers for their burning questions about the trial and the vaccine itself.
What happens on a trial? Is it safe for children? And what happens if you don't like needles?
We put those questions and more to the University of Oxford’s Dr Sean Elias and Dr Grace Li.

Why would I need a vaccine? I thought children didn’t get Covid-19?
Children can get Covid-19, but they seem to get it less frequently and in the majority of cases, it has been much less serious. However, there have been a number of children (the majority of whom had pre-existing medical conditions) who developed serious symptoms when they caught Covid-19 and needed to go to hospital. It’s not fully known just how much children can transmit the disease, but we know it does happen. Offering the vaccine to children will likely help to slow the spread of the disease.
Why are there so many different vaccines?
At the start of the pandemic, all the major vaccine research teams in the world attempted to make vaccines using their preferred methods. There was no way to know if one approach would work better than another, if at all. For a global pandemic we need global supplies of vaccines so several different options is a good thing!
What’s the difference between the different vaccine types?
Newer vaccines such as the Oxford Covid-19 vaccine differ from traditional vaccines in how they activate the immune system. Traditional vaccines inject the antigen (part of the disease that stimulates an immune response) directly into the body. In contrast, newer approaches deliver the genetic instructions for the antigen to the body’s cells. The cells then manufacture the antigen which stimulates the immune response.
What type of vaccine is the Oxford vaccine? What happens in the body when you’re given it?
The Oxford Covid-19 vaccine is known as a ‘viral vectored vaccine’. We use another non-replicating virus to deliver the genetic information for the coronavirus spike protein (a protein on the surface of a coronavirus that allows the virus to attach to a host cell, the main way the virus infects us) directly to our body’s cells.
Our cells make the spike protein and display it on the outside of the cell. This stimulates an immune response, producing T cells and antibodies which protect against coronavirus infection. Antibodies bind to the spike protein on the virus preventing it from infecting cells of the body. T cells destroy cells already infected with the virus.
Is it the same as the vaccine given to adults? Does it work differently on children?
The vaccine we are using is the same as the one given to adults and we are also testing the same dose of vaccine that was given to adults in this study.
Younger children and babies do have a very different immune system to adults and this can affect how strong the immune response to the vaccine is in these age groups. As children get older, their immune system matures, to the point that there are very few differences between older teenagers and young adults.
Does this vaccine work against the newer strains?
The vaccine works well against the UK ‘Kent’ virus strain and we are working to better understand its effectiveness against other strains too. We hope that it will still provide some level of protection, at least preventing hospitalisation.
When a virus mutates it changes a part of itself. Our immune system (T cells and antibodies) may not be able to recognise this specific part of the virus following this change. However, it can still recognise other un-mutated parts of the virus. This is why protection is often reduced but not lost completely. As a backup we are already planning for adjusted vaccines in case they are needed in future.
 Image source, The University of Oxford
Image source, The University of OxfordIs it safe to test vaccines on children? Is it ethical?
Children usually get milder disease than adults but some, especially those who may have other illnesses can still get very sick. Children also spread the virus to others, so vaccinating children is important. Testing vaccines in children is actually very common. The vaccines you will have received as a baby or as an older child will have been tested in clinical trials of the target age groups first to ensure safety and effectiveness before wider use.
The Oxford vaccine has been shown to be very safe in over 24,000 adults. Based on previous experience of our vaccine technology in children, we fully expect the Oxford Covid-19 vaccine to also be safe for young people, but it is important to confirm this using clinical trials.
What sort of person is eligible for this trial, or children’s trials in general? How is it decided?
When selecting the age group of participants in a trial we choose who will benefit most from vaccination. In this study we are looking at healthy children aged six-17, those of school age who we suspect may contribute to virus transmission. Younger children and babies are the least affected by this virus and likely don’t contribute much to virus transmission which is why they are not included in this study.
What happens on the trial?
Children will receive either the Oxford Covid-19 vaccine or a control vaccine for meningitis, called MenB. Everyone will receive two doses of the same vaccine, half receiving the second dose after four weeks and half receiving the second dose after 12 weeks.
Participants and their parents will be asked to complete an e-diary for 28 days after receiving each dose of the vaccine to record any symptoms following vaccination. They will also have five blood tests throughout the study to assess the immune response to the vaccine.
When could vaccines be made available for children?
First, we need to confirm the vaccine is safe and produces a good immune response in children. The good news is, as it is already approved in adults this should help speed up the process.
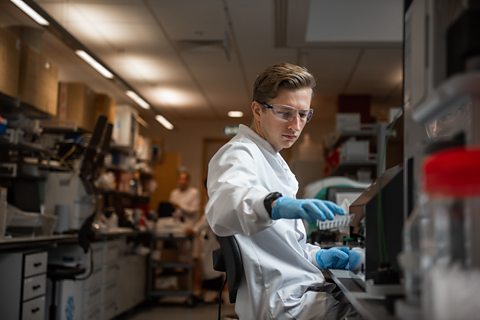 Image source, John Cairns
Image source, John CairnsAre there any options available for people afraid of needles?
Unfortunately, all the available Covid-19 vaccines rely on injection by needle and syringe. Researchers are working on other ways to give children the vaccine which don’t involve a needle and syringe but none of these are ready yet.
What are the side effects to the vaccine?
Because vaccines work by triggering your immune system, you may experience side effects after you receive a vaccine that feel similar to having a real infection. Things like having a fever, or feeling achey, or getting a headache (often described as ‘flu-like’ symptoms) are common after receiving many vaccines and this is the same for the approved Covid-19 vaccines. Other common side effects include a sore arm, chills or general tiredness.
Is it ok for people to take the vaccine if they’ve had allergic reactions in the past?
We recommend talking to a doctor before you have the vaccine. All the ingredients in the vaccine are listed so if you have an allergy to any of these it is not recommended for you to have the vaccine. The Oxford vaccine doesn’t contain any common food allergens (e.g. egg which is found in some flu vaccines). Please ask if you are unsure.
Could taking the vaccine affect my development, or cause disabilities?
Safety is a priority for all vaccines being developed and there is no evidence that any vaccines affect development or cause disabilities. There have been some misleading stories published in the past that vaccines can cause disabilities such as autism. Scientists have repeatedly proved that these stories have no scientific basis.

How long will it take to make a Covid-19 vaccine?
We asked one of the scientists currently researching and trialling a potential vaccine.

Three female scientists whose work is helping us fight the pandemic
Scientists' work from centuries ago, as well as what they're doing right now, is helping us beat coronavirus.
Five Covid-19 vaccine false theories - debunked
You've probably read a lot of things about the coronavirus online, but not everything you have seen is true.
